Tracey Koehlmoos, Linda Kimsey, David Bishai, and David Lane
The Imperative for a Health Systems Approach to Global Health Engagement
12 ìàðòà 2017
The military health system is a strategic asset. The Department of Defense (DOD) spends more than half a billion dollars per year on global health engagement (GHE). There is a shift from an exclusive focus on service delivery to information-gathering in order to support community engagement in public health policy development, thus engaging broader elements of the health system. This transition requires DOD GHE efforts to consider how they can contribute to stronger health systems and broader global health objectives. Military GHE is an essential part of a national strategy that recognizes the importance of strong health infrastructure to the stability and health of nations.1 In the context of competing budgetary concerns within DOD, it is even more essential that GHE not only meets the needs of partner nations but also produces maximum benefit to the broader policy objectives of the United States. Systems engagement is more aligned with U.S. projection of soft power as well as improving civic engagement between American health assets and civil society in partner countries.

President Obama talks with Director of the Centers for Disease Control and Prevention regarding recently diagnosed Ebola case in Dallas, Texas, September 30, 2014 (The White House/Pete Souza)
Expanding Soft Power
In the development and health care arena, both health and/or general systems thinking strives to capture how various elements are connected to each other within the whole. In approaching an issue or an intervention, however discrete, there is the need to model the impact that one change, one input, one circumstance might have on the broader environment. In this context, it is useful to invoke a model showing how things relate to one another. By thinking and engaging with the health system rather than with a single component, the ability exists to produce a synergy in which the outcome of engagement is greater than the sum of the individual parts.2
Evolution of DOD GHE
Although DOD was formally established in 1949, its roots go back to the founding of the Army, Marine Corps, and Navy prior to the American Revolution. Global health projects date back to the Philippines campaign in the late 19thcentury, which attempted to use the delivery of health services to foster support for U.S. forces. During the 20thcentury, the military not only proved that mosquitoes were the vector for yellow fever, but also engaged in prevention programs for yellow fever and malaria. The era after World War II saw the creation of overseas laboratories in Guam, Egypt, and Thailand and the development of the hepatitis-A vaccine. Later in the 20thcentury, in addition to the medical research laboratories, there were efforts to help countries contain biological threats and to assist with the delivery of health services through short-term, episodic medical interventions often referred to generically as medical civic action programs (MEDCAPs) or medical readiness training exercises. Since the United Nations (UN) Security Council’s 2001 declaration that HIV was a national security threat because of the potential destabilization of societies, DOD has deepened its engagement in global health through basic research and development, health service delivery, and public health projects to support a systems response to ongoing and emerging health threats.3
Following criticism for disjointed efforts and lack of progress toward achieving broader engagement objectives, DOD made a series of policy and organizational changes during the past 5 years to adopt a more balanced approach that supports sustainability and demonstrates the effectiveness of such engagement. Perhaps most importantly, the 2010 DOD Instruction 6000.16, “Military Health Support for Stability Operations,” declared that GHE should be given priority comparable to combat operations. DOD is increasingly emphasizing and engaging in GHE activities within the areas of responsibility of each of the combatant commands so that more than 50 percent of DOD’s humanitarian assistance projects, throughout all combatant commands, are medical or health related. However, there is still a lack of clarity in the primary authority over all of DOD GHE activities.4
In 2011, the Under Secretary of Defense for Policy, who has policy but not execution oversight of foreign engagements, established the military position of Global Health Engagement Coordinator within the Stability and Humanitarian Affairs Office. This office provides policy oversight and guidance for conducting health- and medical-related activities with foreign civilian and military entities. The creation of other new offices for coordination includes the Global Health Working Group as well as an International Health Division within the Defense Health Agency. To capture effectiveness of interventions, the department commissioned the Measure of Effectiveness for Defense Engagement and Learning program to develop a method to better evaluate how GHE helps meet U.S. national security goals and establishes a tool to assess efficiency and effectiveness of health engagements.
Understanding the Components of the Health System
The World Health Organization (WHO) defines a health system as “all organizations, people and actions whose primary intent is to promote, restore or maintain health.”5 Traditionally, much of DOD health engagement focused on the delivery of health services by military personnel or, more recently, in collaboration with host-nation military personnel, as opposed to maximizing the potential to build capacity, promote stability, and strengthen relations through engagement with elements of the entire health system. A country’s health system is not the same as a health care system. There is frequently confusion over the connection of health care services with the broader determination of population health in the overall health system.
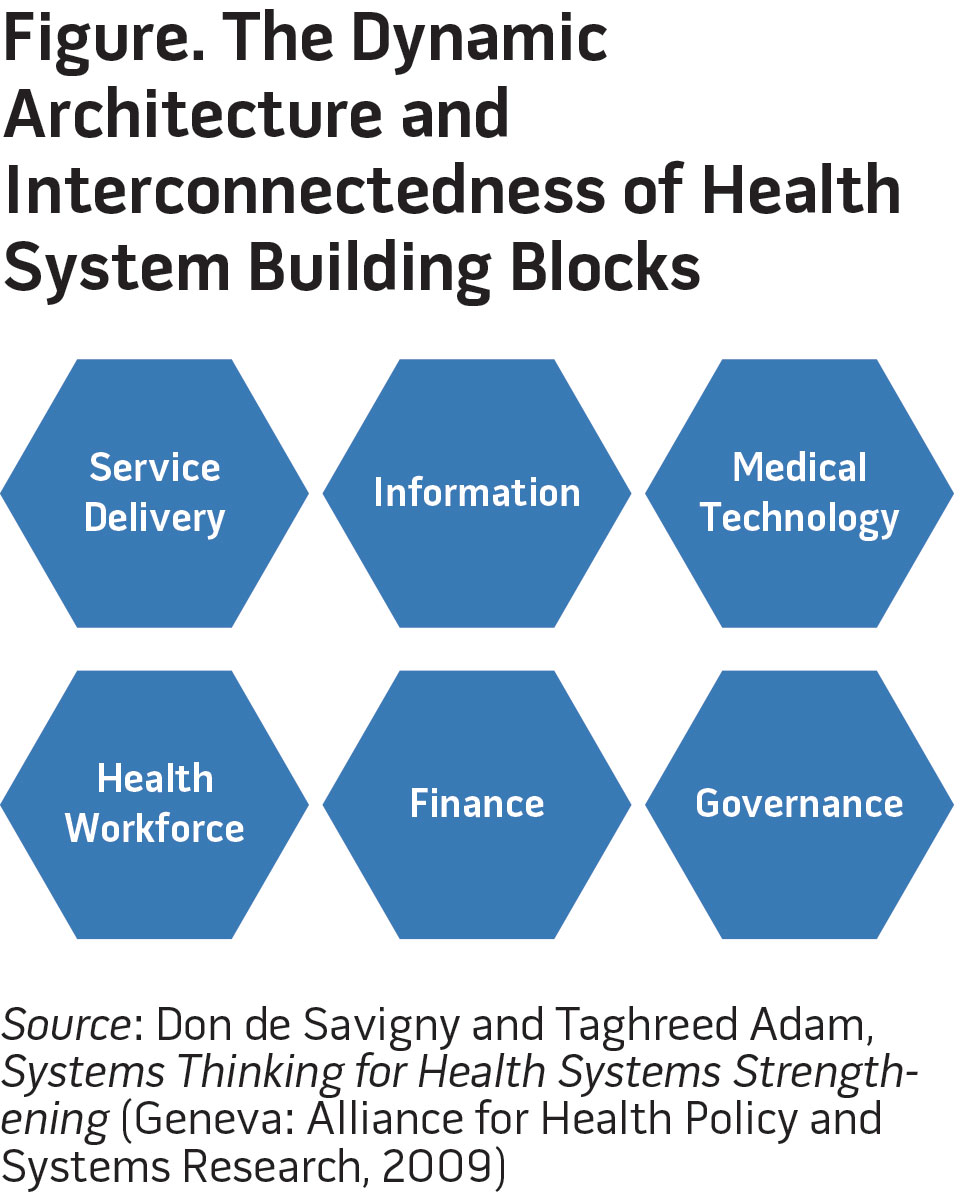
The delivery of health services is just one of six building blocks of the health system, as originally proposed in the WHO’s Framework for Action.6 The other five building blocks of a health system are the health workforce, health information, medical technology, health financing, and leadership and governance (see figure). The six–building block model proposed in the Framework for Action, like other health systems models, provides a conceptual framework toward understanding the entirety of a health system while also facilitating the effective comparative analysis of different health systems around the world. Each building block will be described in turn, accompanied by current and/or potential mechanisms for military health system engagement. An important systems principle is that these building blocks have multiple layers of interconnection and the whole is larger than the sum of its parts. A key concern for DOD is ensuring that its engagement effects the interconnection to create greater coherence and alignment with the objectives of better population health and projection against emerging threats.
Service delivery, almost exclusively direct patient care, has long been a hallmark of DOD GHE. Service delivery includes aspects of packages of services being offered; delivery models like in the home, in the community, or in the clinic or hospital; health infrastructure and flow of logistics; management; safety and quality; and capturing the demand for care.7 This work was most frequently conducted through MEDCAPs and their dental counterparts or as part of a disaster response or humanitarian aid situation.
While the fallback for consideration in service delivery is the government or public sector services, in many low- and middle-income countries a substantial proportion of all health services is actually sought in the nonstate sector. There is growing acknowledgment that governments and donors must look beyond the traditional boundaries of public health service delivery and engage the nonstate sector (that is, private, nongovernmental organizations [NGOs], faith-based organizations, and so forth)—although it is not clear how best to do this—and interventions to work with the nonstate sector may have unintended effects. An example highlighting this change from public to nonstate service engagement from the recent conflicts in Iraq and Afghanistan includes military personnel delivering health services in conjunction with NGOs in Afghanistan. One lesson learned about how best to work with nonstate actors and the possible unintended consequences is to complement rather than duplicate the efforts of other agencies including NGOs. Additionally, local civilian governments, and the health services provided directly to civilians, should emphasize the local standards of care so that unsustainable interventions do not lead to unrealistic expectations or the perception of a decline in “positive perceptions of the U.S. military.”8
The health workforce is the next building block. It is made up of the people within a country whose primary role is to protect and/or improve health regardless of level of training. There is great variation in the type and density of cadre, especially in developing countries. Viewed as a spectrum, there might be physicians, policymakers, planners, and managers at one end and skilled birth attendants, community health workers, and even untrained providers and drug sellers at the other—spread between the public, nonstate, and private sectors. WHO has found a strong positive correlation between health workforce density and service coverage and health outcomes.9 GHE in the health workforce building block might include augmenting the training programs of partner-nation military physicians by visiting U.S. military physicians. In a newer expanded paradigm of health engagement, corpsmen might share skills with community health workers or via short-term exchange programs at medical, dental, health service administration, and nursing schools.10 Of note, however, lessons learned from Afghanistan have demonstrated that investment in medical and educational infrastructure without assuring that the local health workforce and health system can sustain new facilities should be avoided.11
Next, information means that the health system allows the generation and strategic use of information, intelligence, and research on health. Ideally, three areas should be covered under health information, including data and analysis on health determinants, health systems performance (including outcomes), and health status of populations. Some well-developed examples of GHE that support this building block include the development of disease surveillance systems, the rollout of standardized and reliable tools and instruments, and the collation and participation in the publication of international health statistics. The WHO states that “more than just a national concern, as part of efforts to create a more secure world, countries need to be on the alert and ready to respond collectively to the threat of epidemics and other public health emergencies.”12 A functioning health information system in a country enables local and global decisionmakers to prevent or respond to a crisis in a real-time manner. Partner nations can be empowered to collect, analyze, and share their own health information. This type of engagement is longstanding to some extent through the Centers for Disease Control’s (CDC’s) Global Health Security Branch and especially the joint Biological Threat Reduction Program as well as through the network of military laboratories led by the Armed Forces Health and Surveillance Center. Moving forward, however, efforts should be made to build capacity in the host nation and empower local institutions strengthening the relationship between nations rather than just train local employees to support the U.S. military–led efforts in a nonsustainable manner.

Patients wait during Medical Civic Action Program in Lunga Lunga, Kenya, August 23, 2012, as part of Combined Joint Task Force–Horn of Africa (U.S. Air Force/Daniel St. Pierre)
The next building block is medical technology. Broad areas within this building block include medical products, vaccines, and other technologies with a cross-cutting emphasis on quality, safety, and cost-effectiveness of these items. To some extent, DOD could participate in the technology transfer from high-income countries to developing countries with an emphasis on essential medicines for maternal child health and neglected tropical disease. DOD work on vaccines is perhaps its most visible contribution to global health, having played a major role in developing 25 percent of all licensed vaccines in the United States since 1962. More recently, DOD has led the only late-stage clinical trials for vaccines found to be efficacious against malaria and HIV. While the Army and Navy’s overseas medical research laboratories in Thailand, Egypt, Peru, Kenya, Germany, and Cambodia conduct medical research that ties directly to the protection of deployed Servicemembers, their work has led to the development of health products including vaccines, drug therapies, and medical devices with the ability to improve health worldwide, as well as building the local medical and scientific capacity.13 One recent accomplishment is the successful development and testing of an HIV vaccine in Thailand. Consistently low funding for the laboratories has led to the creation of entrepreneurial scientific activities with local and global partners such as universities and other international agencies, thus strengthening the brand and, in most cases, the relationship with local governments, so the labs should be considered “national assets.”14 However, as exemplified by Naval Medical Research Unit 2, whose 40-year history in Indonesia ended in 2009 during a protracted and aggressive disagreement over viral sample rights to H5N1 (Avian Influenza), it is essential for these facilities to protect their work and the U.S. Government’s investment through the development and maintenance of host-nation champions.15
The penultimate building block is financing. Health financing mechanisms vary across nations depending on history, institutions, and traditions. The goal of health financing should be to reduce gross inequities in access to necessary care and avoid catastrophic costs to the population, especially the poor. In some developing countries, there are innovative approaches like micro-insurance, voucher schemes, or social franchising in efforts to provide universal coverage. There is no one best or right model, but the military health system should be cautious not to deliver services that diminish confidence in or otherwise interrupt local programs and practices.
While the financing of the health sector may appear to be the health systems building block best suited to be addressed by other agencies in the U.S. Government, DOD contributes to this effort, too. For example, DOD engagement helps in the fight against HIV through implementation of the President’s Emergency Plan for AIDS Relief (PEPFAR), which in general supports work in 73 countries. PEPFAR supports HIV/AIDS prevention, treatment, and care, strategic information, development of human capacity, and development of programs and policies in partner militaries and civilian communities. Thirteen PEPFAR countries have unique military-to-military–specific HIV/AIDS prevention programs designed to address risk factors, in addition to treatment and care programs for their personnel. It is worth noting that the DOD budget for fiscal year 2011 for PEPFAR was $148.5 million, and most of these accounts are administered by combatant commanders or the Defense Security Cooperation Agency. The DOD HIV/AIDS Prevention Program is a relatively small portion of PEPFAR funding and is stovepiped from the broader health systems finance. While efforts toward health sector reconstruction in Afghanistan might serve as an example of health financing, DOD has limited engagement in this arena but can seek to improve in future efforts.
Last and perhaps most importantly, the building block of leadership and governance is the most complex. Also known as stewardship, this area focuses on ensuring strategic policy frameworks and effective oversight of the system; coalition-building; and accountability, regulation, and attention to the overall design of the health system.16Again, there is no single model for stewardship of a health system, although in most countries the default is to the ministry of health or its equivalent. However, before the military engages in global health, consideration should be given to the reality that in some developing countries, there are large-scale NGOs serving a majority of the population. For example, in Bangladesh the NGO BRAC (formerly known as the Bangladesh Rural Advancement Committee) has more than 64,000 village health workers who touch the lives of 110 million Bangladeshis and, as the world’s largest NGO, has more than 120,000 employees working in 14 countries including Afghanistan, Uganda, Pakistan, and Sudan.17 A long-term gap in this area was that humanitarian visits by U.S. Navy hospital ships often took place with little if any interaction with local health-related activities undertaken by U.S. civilian agencies and NGOs.18 Furthermore, military GHE with host-nation leadership appears to lack clear guidance as to which agency (U.S. civilian or host nation) should engage local governments, and there appears to be no consistent guidelines on when to depart a humanitarian relief situation. Efforts to develop defense health leaders from foreign nations require research in terms of effectiveness for improving GHE and strengthening health systems.
Critical Considerations for Expanding Soft Power
Unintended consequences and connections typify health systems, and policymakers and strategists must design monitoring systems and stakeholder engagement to remain responsive and proactive. Such holistic thinking and broad objectives could assist with overcoming the pervasive misunderstandings in the approach, culture, and vocabulary that currently hamper the DOD ability to work well with other agencies and groups in the global health arena.19 Given the prominence of GHE as a key to soft power for the United States, more effort should be given to achieving sustainable, well-planned, and well-coordinated military-to-military and military-to-civilian activities.20Furthermore, in the current Joint Concept of Health Services, although its primary focus is on the readiness of U.S. medical forces, GHE is encouraged with an eye toward assisting partner nations to develop and sustain their health service networks to ensure capabilities are suitable, accessible, and understood when the United States needs them to support operations. Better engagement would enable DOD actors to use existing resources to understand both the health system of the partner nation and the evidence base for an appropriate response. These resources exist in places such as the WHO-sponsored Asia Pacific Observatory on Health System and Policy, which is home to Health System in Transition reports and the Evidence Aid repository, which is an international initiative to provide information to decisionmakers through creating access to systematic reviews on the effects of interventions and actions of relevance before, during, and after natural disasters and other humanitarian emergencies.
Health Systems and National Objectives for Future GHE
Future engagement by the military with international governments and health systems might benefit from closely aligning with broader national and international models. Some examples of effectively using soft power to improve the health of the poor might include assistance with achieving specific targets in the Millennium Development Goals and the forthcoming Sustainable Development Goals, which will include responding to the emerging threat of noncommunicable diseases and assistance with stemming the scourge of motor vehicle crashes. Developing capacity in these areas demands engagement across multiple sectors of government and civil society. Public health practitioners in partner countries in connection with public health experts from DOD could and should convene local stakeholders from law enforcement, commerce, transport, and the private sector to examine epidemiological data on modern threats to health.
First, the majority of low- and middle-income countries have spent the previous 15 years engaged in efforts to achieve the UN Millennium Development Goals. There are well-evidenced packages of interventions for achieving most of the health-related goals, such as reducing infant mortality, improving maternal health, and combating HIV/AIDS, malaria, and other devastating infectious diseases. Future MEDCAPs or training exercises could work with partner nations’ ministries of health or local NGOs to understand the country-specific, targeted approaches required to achieve the goals and to ensure that all health services assisted with meeting the goals. An example of this is providing and promoting the use of zinc in the treatment of childhood diarrhea in partnership with host-nation efforts to scale up such intervention to reduce child mortality.
Another example of potentially relevant engagement that is of concern to both partner nations and DOD is traffic-related deaths. It is predicted that by 2030, traffic injuries will be the fifth leading cause of death. Already approximately 1.3 million people die due to traffic accidents each year, and an additional 20 million to 50 million are injured or disabled. Despite being home to fewer than 50 percent of the world’s motor vehicles, low- and middle-income countries have 90 percent of the mortality burden for traffic accidents.21 Traffic deaths are also a risk to U.S. Servicemembers while on deployment or otherwise serving abroad. Thus, there is the possibility of direct benefit to the United States through engagement that promotes and implements proven interventions such as driver training, traffic calming mechanisms, and others that could lead to a reduction in the amount of traffic deaths and injuries.22 Such engagement might come through exposure and diplomatic engagement with high-level policy leaders in a cross-sector setting such as transportation and urban planning in addition to health, or it might come through sharing driver safety programs for cars and/or motorcycles, like those used by DOD. Best practice in this area looks like a cross-governmental task force with ongoing expertise in surveillance of rates of crashes, injuries, deaths, speeding, seatbelt use, helmet use, and drunk driving. A good response includes all aspects of a health system that is much broader than clinical service delivery. The shift in global epidemiology has raised issues such as road safety and noncommunicable diseases to the forefront, and it is incumbent for DOD policymakers and strategists to adapt to this change.

Patient looks through lens to determine eyeglass prescription during 2013 Operation Pacific Angel, Dong Hoi, Quang Binh Province, Vietnam (U.S. Air Force/Sara Csurilla)
Conclusion
Innovation often occurs during tragedy. The Ebola epidemic in western Africa in 2014 took steps toward exemplifying a whole-of-government health systems strengthening approach to GHE, particularly in Liberia. DOD provided an investment and committed military personnel to permanent infrastructure development, the U.S. Agency for International Development committed to train local providers, the U.S. Public Health Service sent health care providers, the CDC and DOD provided disease surveillance, and broad coordination occurred across U.S. agencies that included international and local NGOs. The U.S. Government committed $750 million toward the response, although the real total is likely to be considerably higher by the end of the engagement.
Such comprehensive approaches to the health systems building blocks, however, would benefit all manner of future global health engagements. DOD should work to capture best practices in health systems engagement so that it can move away from the days of poorly designed health activities that failed to coordinate with local governments and providers and led to little enduring benefit for the host nation or diplomacy.23 The recent push toward organizational structure and programmatic support, as well as the development of models to capture effectiveness, are steps in the direction toward maximizing soft power from GHE.
Recent policy and structure changes within DOD lend themselves to taking a health systems approach and promote an ease of collaboration as highlighted during the response to the Ebola epidemic. Such steps are indeed promising, but a health systems approach and systems thinking that recognize the interaction between building blocks and incorporates service delivery, the health workforce, health information, medical technology, health financing, and leadership and governance should become a hallmark of all future DOD GHE. If it is true that for every $1 spent on diplomacy and development, $5 is saved in defense, then there is an even greater imperative to efficiently and effectively use the military for promoting diplomacy. However, DOD GHE should be aligned to policies, priorities, and perspectives among partner-nation policymakers, strategists, and agencies, as well as among international agencies to engender collaboration, cooperation, and stability. JFQ
Notes
1 Aizen J. Marrogi and Saadoun al-Dulaimi, “Medical Diplomacy in Achieving U.S. Global Strategic Objectives,” Joint Force Quarterly 74 (3rd Quarter 2014), 124–130; David Smith, “The DOD and Global Health Engagement,” USMedicine.com, October 2014, available at <www.usmedicine.com/agencies/department-of-defense-dod/the-dod-and-global-health-engagement/>.
2 Don de Savigny and Taghreed Adam, Systems Thinking for Health Systems Strengthening (Geneva: Alliance for Health Policy and Systems Research, 2009).
3 Joshua Michaud, Kellie Moss, and Jennifer Kates, U.S. Global Health Policy: The U.S. Department of Defense and Global Health (Washington, DC: Kaiser Family Foundation, 2012).
4 Ibid.
5 World Health Organization (WHO), Everybody’s Business: Strengthening Health Systems to Improve Health Outcomes—WHO’s Framework for Action (Geneva: WHO, 2007).
6 Ibid.
7 Ibid.
8 J. Christopher Daniel, Global Health Engagement: Sharpening a Key Tool for the Department of Defense (Washington, DC: Center for Strategic and International Studies, 2014).
9 WHO, Everybody’s Business.
10 Aizen J. Marrogi, J. Fike, and Edwin Burkett, “The Role of Graduate Medical Education in the U.S. Global Health Engagement Effort,” poster presented at Association of Military Surgeons of the United States, Washington, DC, December 2, 2014.
11 Daniel.
12 WHO, Everybody’s Business.
13 J. Stephen Morrison et al., The Defense Department’s Enduring Contributions to Global Health: The Future of the U.S. Army and Navy Overseas Medical Research Laboratories (Washington, DC: Center for Strategic and International Studies, 2011).
14 Ibid.
15 Ibid.
16 WHO, Everybody’s Business.
17 Tracey Pérez Koehlmoos et al., “Health Transcends Poverty: The Bangladesh Experience,” in “Good Health at Low Cost” 25 Years On: What Makes a Successful Health System? ed. Dina Balabanova, Martin McKee, and Anne Mills (London: London School of Hygiene and Tropical Medicine, 2011).
18 J. Stephen Morrison et al., U.S. Navy Humanitarian Assistance in an Era of Austerity (Washington, DC: Center for Strategic and International Studies, 2013).
19 Michaud, Moss, and Kates.
20 Marrogi and al-Dulaimi.
21 WHO, “Fact File: 10 Facts on Global Road Safety,” available at <www.who.int/features/factfiles/roadsafety/facts/en/index.html>.
22 Tracey Koehlmoos, Shahela Anwar, and Alejandro Cravioto, “Global Health: Chronic Diseases and Other Emergent Issues in Global Health,” Infectious Disease Clinics of North America 25, no. 3 (September 2011), 623–638.
23 Morrison et al.
Âåðíóòüñÿ íàçàä