Kyle N. Remick and Eric A. Elster
Trauma Care in Support of Global Military Operations
15 ñåíòÿáðÿ 2017
Colonel Kyle N. Remick, USA, MD, is the Military Deputy of the Combat Casualty Care Research Program at the U.S. Army Medical Research and Material Command, Fort Detrick, Maryland. Captain Eric A. Elster, USN, MD, is Professor and Chairman of the Department of Surgery at the Uniformed Services University of the Health Sciences and the Walter Reed National Military Medical Center.
June 20, 2017 — The Department of Defense (DOD) Joint Trauma System (JTS) revolutionized combat casualty care by creating a trauma system for the battlefield. Over the past 30 years, U.S. civilian trauma systems have decreased mortality from trauma by 15 to 20 percent.1 In 2006, senior military and civilian medical leaders partnered to translate this civilian model to the battlefield. The deployed components of the JTS provided real-time data collection and analysis, research to guide rapid implementation of knowledge and material products, clinical guidelines for optimal care, and direct guidance to commanders as a key components of a continuously learning trauma system in two theaters of operation, directly saving lives on the battlefield.2

Senior Airman provides dental care as member of 59th Dental Support Squadron, providing high-performance health system dedicated to excellence in global dental care and education, Base San Antonio–Lackland, Texas, January 26, 2016 (U.S. Air Force/Keith James)
The JTS must now adapt to similarly support new challenges posed by dispersed and globally remote operations outside of formal combat zones and with fewer dedicated medical resources. In this context, developing regionally relevant trauma care system strategies has the potential to decrease mortality from injury for this new global operational environment. The creation of this global trauma care system strategy requires the synergy of four trauma-oriented pillars of effort. These are global trauma care, medical interoperability, medical stability operations, and health diplomacy. Their importance and unique contribution to an overall global strategy of trauma care is described.
Global Trauma Care
From a trauma systems and medical operational perspective, the term global trauma care implies the scenario distinct from combat operations in a mature theater of war in which all roles of care and extensive military resources are not necessarily available. With numerous, small scale, and globally dispersed operations currently ongoing and over the horizon, a plan of action to provide trauma care for serious injuries is of paramount importance.
DOD seeks to support all missions with U.S. military trauma resources as close to a 1-hour window as possible as survival from trauma is time sensitive. Where this is not possible, an alternative is to leverage trusted or previously validated partner-nation (PN) military trauma resources. Unfortunately, the reality is that we will not always have the ability to dedicate our own or PN military trauma resources to support all operations.
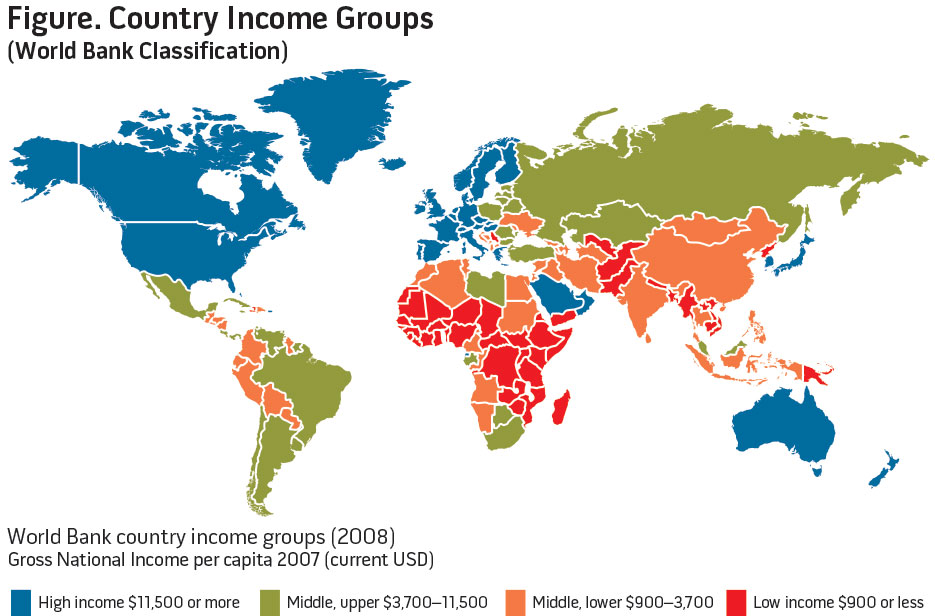
Thus, DOD will need to leverage the trauma capabilities of geographically relevant PNs. This strategy presents several challenges. First, these operational environments are likely to be in low- and middle-income countries (LMICs). Second, these military operations in need of trauma support are likely to be in remote locations. Lastly, the civilian trauma centers and trauma systems in these countries, if they exist, may not deliver care to an acceptable standard for use by Servicemembers. Using the medical care in LMICs as part of our global strategy for trauma care without prior planning would be disastrous and would potentially increase morbidity and mortality.
There is already tangible proof for the need to develop PN trauma capabilities. In December 2013, South Sudan, the world’s newest nation, experienced a rekindling of internal strife in the form of armed conflict between the military of the legitimate president and rebels in support of the former vice president. On December 21, four Servicemembers were injured during an attempt to evacuate American citizens from the town of Bor in the state of Jonglei, approximately 125 miles from the nation’s capital of Juba. Ospreys were damaged in the attempt, but fortunately the aircraft were still able to reach Entebbe, Uganda. The injured U.S. personnel were then transferred to a C17 and transported to a hospital in Nairobi, Kenya.3 After receiving care in Nairobi, the Servicemembers were then evacuated through Landstuhl Regional Medical Center in Germany to the United States.
South Sudan is a low-income country, and its medical infrastructure, to include trauma care, is far below what we would accept for our Servicemembers. Thus, neither the civilian nor the military hospitals in South Sudan would have been an acceptable option for care.4 The Servicemembers were taken to a hospital in Nairobi, which is approximately 745 miles away. This took around 3 hours including the transfer of the wounded in Uganda from the Osprey to the C17. The pre-hospital time was far longer than the now commonly accepted and expected “golden hour” guideline to reach initial surgical care. Furthermore, the Servicemembers were injured on the same aircraft that served as the evacuation platform, so they did not have to wait for a separate medical evacuation, which would have added significantly to the pre-hospital time. The conclusion is the distance to acceptable trauma care was prohibitive. Remote sites with prolonged evacuation times are a challenge for contingency planning, thus supporting the need to develop regionalized PN trauma centers.
The next politically charged question is whether the quality of trauma care in Nairobi is acceptable for our Servicemembers and, more broadly, whether the quality of trauma care provided in any LMIC is acceptable. In general, the answer is no. Thus, multiple options to provide optimal injury care include placing U.S. trauma resources within 1 hour of every military operation, forward-staging air evacuation assets to cover all military operations within 1 hour, or identifying regional PNs and develop their trauma care to a level acceptable for our use. Each of these options has a role in short-term planning to close this gap in trauma care, but the most feasible long-term solution is the third option.
The harsh reality is that we operate in many remote areas of the globe considered to be LMICs (see figure), but with a dedicated, long-term commitment to these LMIC PNs, the care provided could be improved to an acceptable level for our Servicemembers to mitigate risk of death and disability from injury.
Again, this will be a large effort requiring a long-term commitment, but we anticipate this as a major gap in trauma care that will take a combined effort between DOD, Department of State, and other U.S. agencies to resolve over the next several decades. With the assistance of the medical leadership from the U.S. regional military commands, a joint and unified geographic trauma system plan could be developed for each area of responsibility. Strategically located PN civilian or military trauma centers could be identified for development.
Medical Interoperability
The U.S. military may more often partner with North Atlantic Treaty Organization (NATO) nations and others in support of future combat and noncombat operations. In the context of providing trauma care, it is essential to enable resource interoperability between nations to ensure a baseline. Interoperability leverages trauma care as a force multiplier for future limited-resource operational environments. This will be a military-to-military partnership with other nations that will require DOD and Military Health System support for success. The U.S. military has already begun to build relationships with the medical corps of other nations, and there are several examples regarding the benefits of interoperability from recent conflicts from Afghanistan. These examples highlight that successful collaboration relies heavily on predeployment preparation.
Example 1: UK Role 3 Hospital at Camp Bastion. Probably the best example of interoperability within NATO was the United Kingdom (UK) Role 3 Hospital in Camp Bastion, Afghanistan, in support of the British Operation Herrick. Beginning in June 2009, the U.S. Navy was asked to contribute personnel to this facility. This transitioned to the U.S. Army in 2012 prior to closure of Camp Bastion in September 2014. The UK Role 3 Hospital at the camp was rightfully the shining star of the UK Medical Corps and a model for success in medical interoperability.
Early on, the UK established a thorough predeployment training and validation model. This model fully incorporated U.S. medical personnel deploying with British medical personnel in support of the Role 3 Hospital. As with any multinational military endeavor, there are always differences in tactics, techniques, and procedures (TTP). In this case, there were distinct differences in medical TTPs within the hospital command and control procedures and in the practice of trauma care between the United States and UK. In the vast majority of cases, these differences were not better or worse—just different. These differences in roles and responsibilities and in clinical medical practice were clarified in advance of deployment to ensure trust, cooperation, and smooth interoperability among international colleagues.
The UK military medical field exercise Hospex served to facilitate interoperability. The exercise was as the culmination of a successful predeployment training and validation model. Inside a warehouse on a small UK base in the quiet town of Strensall, near York, England, stood an exact replica of the Bastion Role 3 Hospital. A fully experienced and trained staff hosted a week-long validation exercise covering all aspects of Role 3 command and control procedures, patient care in the emergency department, operating room, intensive care unit, and patient ward; management of multi-casualty and mass casualty scenarios; patient evacuation procedures; and detained personnel procedures. After a thorough testing period, the UK military hospital team was validated for Operation Herrick. This predeployment medical field exercise also served as predeployment interoperability training between the UK and the United States. This successful example is a model that we should replicate for future operations.
Example 2: Spanish Role 2 Hospital in Herat. Spain and Italy supported combat operations in western Afghanistan for a decade. Spanish Role 2 was the largest trauma facility in Regional Command–West. Beginning in January 2010, the U.S. military placed surgeons at this facility. Although not as deliberately planned, this partnership was a good example of a NATO partner assuming primary responsibility for trauma care in a specific region of a combat zone. The presence of American military surgical teams in this Spanish facility serves as another example of the need for interoperability.
Example 3: Italian Role 1 in Conjunction with Surgical Team Support of Special Operations. In 2008, a U.S. military surgical team was tasked to support a special operations mission at an Italian base in Afghanistan. The Italian military had an existing Role 1 facility with a primary care physician and medics to provide initial trauma care. The mission of the U.S. Role 2 surgical team was to augment the Italian team’s capability for a short time period while American forces were in the area conducting operations. The U.S. Role 2 successfully supported this brief special operations mission, but prior combined training with the Italians would have yielded a stronger unity of effort.
With the potential for numerous, dispersed operations throughout the world, placement of U.S. military trauma assets in all locations simultaneously may not always be possible. Our goal should be to collaborate and develop interoperability with all of our NATO Allies in order to share the responsibility of providing care. In addition, we should seek out opportunities to collaborate with medical units from less-developed partner nations.

Lieutenant Commander Justin Dye, right, and Dr. Minh Hoaug Vo operate on patient’s spine during Pacific Partnership 2017 in Da Nang, Vietnam, May 2017 (U.S. Navy/Madailein Abbott)
Medical Stability Operations
Partnering to improve host-nation trauma care in support of its security forces is a component of medical stability operations. For success, this effort involves military-to-military, military-to-civilian, and civilian-to-civilian partnerships involving DOD, Military Health System, civilian university and hospital institutions, and Department of State.
In support of stability and security operations and counterinsurgency operations, DOD often supports infrastructure development in key PNs. As an important component of this greater strategy, our military trauma system leadership should collaborate with PN medical leadership in order to develop their trauma system infrastructure. The purpose of this collaboration and development is not specifically for the purpose of caring for injured U.S. Servicemembers but for improving host-nation trauma care in support of its security forces. JTS, as the DOD enterprise responsible for military trauma care, can achieve this through leadership, guidance, and direct development of the host-nation’s trauma infrastructure and capability. This effort has the potential to bolster the host nation’s will to fight and convey a significant psychological advantage to security and counterinsurgency forces in direct support of the overall National Security Strategy.5
This pillar truly overlaps with national global health engagement (GHE) efforts. This uniquely leverages JTS for GHE in operations other than war. A coherent plan for trauma system development for the host-nation security forces should be integrated into the overall plan when conducting operations. The application of JTS to GHE for medical stability operations leverages U.S. military trauma expertise to augment the other means of U.S. power (that is, diplomatic, informational, and economic).
Health Diplomacy
Health diplomacy can represent a variety of activities from formal treaties to multiple stakeholder agreements to informal collaborations.6 Thus, health diplomacy conducted on an informal level by individual DOD organizations must first serve U.S. national interests. Regarding strategic efforts for global trauma system development as part of health diplomacy, it is expected that regional commands would guide these efforts to locations of the military and national security interests. Concurrently, DOD investment in global trauma system development, as a component of GHE, has the potential to provide a measureable benefit to an overall strategy.
As the United States moves forward in GHE, we must be sure that we can measure the effects of our actions. Health diplomacy must not only serve national interests but also provide a measureable benefit to the target of GHE. Furthermore, trauma system development is not mutually exclusive of the other important pillars already discussed. This pillar builds on the previous two involving the JTS role in trauma system advisory and development in LMICs of importance to national security interests.

Tactical critical care evacuation team nurse (forefront) assigned to Army’s 3rd Platoon, C Company, 2-149 General Support Aviation Battalion Medical Evacuation, prepares for patient transfer mission, May 13, 2013, at Forward Operating Base Orgun East, Afghanistan (U.S. Air Force/Marleah Miller)
Conclusion
We stand ready for a changing world that will require revolutionary change in how we wield combat power and how we measure military success. Military success may be measured as much by its finesse as a tool for national security as by its strength. To succeed in this new operational environment, our military medical support must be adaptive, innovative, and exploit the initiative to leverage our recent trauma experience and expertise to enhance direct support to warfighters and augment diplomacy.
Regional combatant commanders will drive the need for a global strategy for trauma care. Their theater security plans will be essential to identify partner nations with the greatest potential to institute sustainable trauma system development. We recommend that the Joint Staff and Services support and encourage this strategy to provide an optimal system for casualty care in support of a globally responsive and regionally relevant joint force. JFQ
Notes
1 Ellen J. MacKenzie et al., “A National Evaluation of the Effect of Trauma-Center Care on Mortality,” The New England Journal of Medicine, vol. 354 (January 26, 2006), 366–378; Avery B. Nathens et al., “A Resource-Based Assessment of Trauma Care in the United States,” Journal of Trauma: Injury Infection, and Critical Care 56, no. 1 (January 2004), 173–178; N. Clay Mann et al., “Systematic Review of Published Evidence Regarding Trauma System Effectiveness,” Journal of Trauma: Injury Infection, and Critical Care 47, no. 3 (September 1999 supp.), S25–S33; Gregory J. Jurkovich and Charles Mock, “Systematic Review of Trauma System Effectiveness Based on Registry Comparisons,” Journal of Trauma: Injury Infection, and Critical Care 47, no. 3 (September 1999 supp.), S46–S55.
2 Brian J. Eastridge et al., “Trauma System Development in a Theater of War: Experiences from Operation Iraqi Freedom and Operation Enduring Freedom,” Journal of Trauma: Injury Infection, and Critical Care 61, no. 6 (December 2006), 1,366–1,373; Brian J. Eastridge et al., “Utilizing a Trauma Systems Approach to Benchmark and Improve Combat Casualty Care,” Journal of Trauma: Injury Infection, and Critical Care 69, no. 1 (July 2010 supp.), S5–S9.
3 Craig Whitlock and Sudarsan Raghavan, “Four U.S. Troops Injured During Evacuation Mission in Strife-Torn South Sudan,” Washington Post, December 21, 2013.
4 Kyle N. Remick et al., “Development of a Novel Global Trauma System Evaluation Tool and Initial Results of Implementation in the Republic of South Sudan,” Injury45, no. 11 (November 2014), 1,731–1,735.
5 Ramey L. Wilson, “Building Partner Capacity and Strengthening Security Through Medical Security Force Assistance” (Ph.D. diss., Naval Postgraduate School, 2013).
6 Rebecca Katz et al., “Defining Health Diplomacy: Changing Demands in the Era of Globalization,” The Milbank Quarterly 89, no. 3 (September 2011), 503–523.
Âåðíóòüñÿ íàçàä